Prolapse uterus and it's entangled factors: her story is Nepal's story
Smriti Suwal, Nepal
Senior training officer, physiotherapist
Among the stories of various women with prolapse uterus, the story of Maya Gurung (name changed) was heart wrenching. Her story shows how isolated and deprived the Nepalese Women are. She had a first degree prolapse at the age of 20 and had been living with it till now. Her story says how responsive our health and social system is? I believe her case represent many Nepalese women living in various districts and villages of Nepal.
There are specific rehabilitation protocols for the prevention and rehabilitation for prolapse uterus and fistula. Many health workers are aware of Kegel exercise and thanks to previous training programs to these health workers. The concept of exercises is always emerging and changing as per new researches and so does apply for Kegel. On top of all, without the correct demonstration and confirmation of perineum contraction, Kegel’s are most often wrong and that gives opposite effect. Also programming the Kegel exercise technique on daily activities like lifting the load is very important to prevent the stress on pelvic floor. Importantly, there are specific doses and implications for strength and endurance for pelvic floor muscle that needs to factored in while designing Kegels. My experience says that for Nepalese women, intervention focused at minimizing the risk of pelvic floor stress by teaching the safe way of performing household chores is the most important preventive method.
Let’s come to Maya Gurung. She had suffered from first degree uterus prolapse during her first post-partum phase, 30 years back when she had delivered her first son.
Immediately after delivery, she had to carry heavy water pots and heavy wood and walk for an hour which resulted in first degree uterus prolapse. She thought that’s a minor problem and did not feel like seeking the service from health facility which is 7 hours walking distance from her village. For her, priority was household activities rather than seeking the treatment. Neither her husband nor family insisted her to visit the health facility. This made the situation worse and aggravated to third degree prolapse. Now she has complications like incontinence and abnormal vaginal discharge which is degrading her health and self-esteem.
Now Maya says “I have difficulty on defecation, feels like I am dying with the pain”. Her day starts from 2 am in the morning to carry cattle fodder and carry water pots from a mile. It’s sad that she has compulsion to continue her activities of daily living with difficulties. She felt that she is not getting cured and won’t live longer. This feeling has made her more depressed and stressed. With her eyes full of tears says “I am worried about my youngest daughter who is studying in grade 7th as she is the most precious part of my life”. I was surprised to know that her husband is a drunkard who rather than lending helping hands, snatches her money for gambling. She has a small farm and this has been her source of income to run a family but her ideas and thoughts are not taken for family decision making. Her degrading health situation has left her low esteemed that’s why she does not prefer to participate in community functions and decision making events.
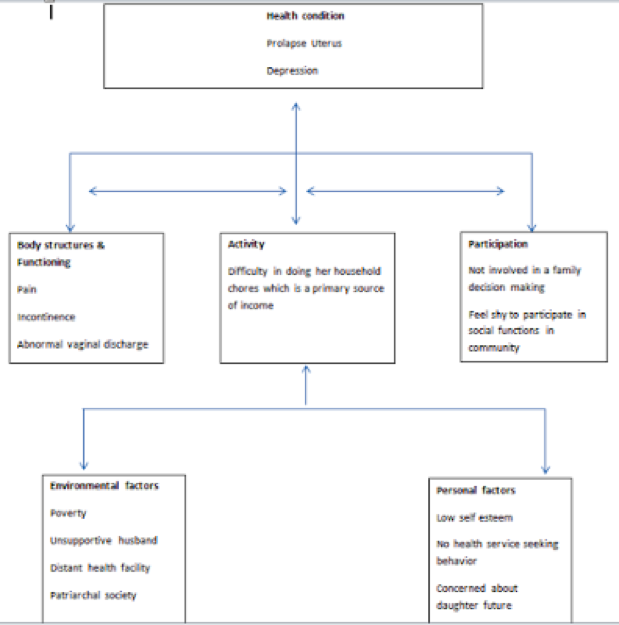
Let’s assess Maya using the International classification of functioning (ICF) model
The main barriers for her was poor health seeking behavior which is linked to her and family illiteracy and poverty level. Another one is distant health facilities that also further contributed to her non health seeking behavior. The third one is our patriarchal culture in which women are confined within the household chores which are stressful. In a course of time, these three factors contributed for degrading health, low activity level and participatory restriction in Maya’s life.
Maya’s story clearly depicts that uterine prolapse is not only a health problem but it is entangled with many issues like education, empowerment and economy of family. Therefore, a mutisectorial, inter/intra departmental and inter/intra ministerial approach is a must.
This was the health camp where I participated, soon Maya will undergo hysterectomy. But her other barriers will still remain the same that may further bring complications like urinary incontinence and vault prolapse. Her husband is still not supportive, her poverty line is still the same and she still has compulsion to do heavy household works. There are many Mayas in Nepal who are living below poverty line. Isn’t it the time to think? Isn't it the time to utilize the long experience (available data and lesson learnt) to design the sustainable solutions?
Being a physiotherapist, I feel honored to meet Maya and understand the situations of women living with prolapse in Nepal. I know that my contributions to bring Maya to good living situation through my physical therapy intervention are just like a drop in Ocean. Despite of all these, i am hopeful that i was able to contribute at least a new and very important drop in the ocean, the thing that has never started before (Rehabilitation component added to prolapse uterus management). This has definitely ensured a multidisciplinary approach of care. Maya, now knows how to do her activities with minimal stress on her pelvic floor and what relieving position/exercises to do if she experiences a sudden difficulty. Again she will require physical therapy intervention after surgery to prevent the complications like incontinence and vaginal vault prolapse.
Nepal has 1800 physiotherapists but not more than 20 quotas are allocated by ministry of health in the health system. Ministry of health has Nepal health sector strategy, national prolapse uterus management guideline, and health worker training manual for fistula and prolapse uterus management, national childhood disability management strategy, birth defect surveillance and control plan as the guiding documents that strongly support to have physiotherapist in a health system. Also there are sufficient human resources in the country now. At this favorable situation (where human resources are available to fulfill the service demands), Nepal should not make any delays to deploy physiotherapists into the health system.